Pacing Maneuvres
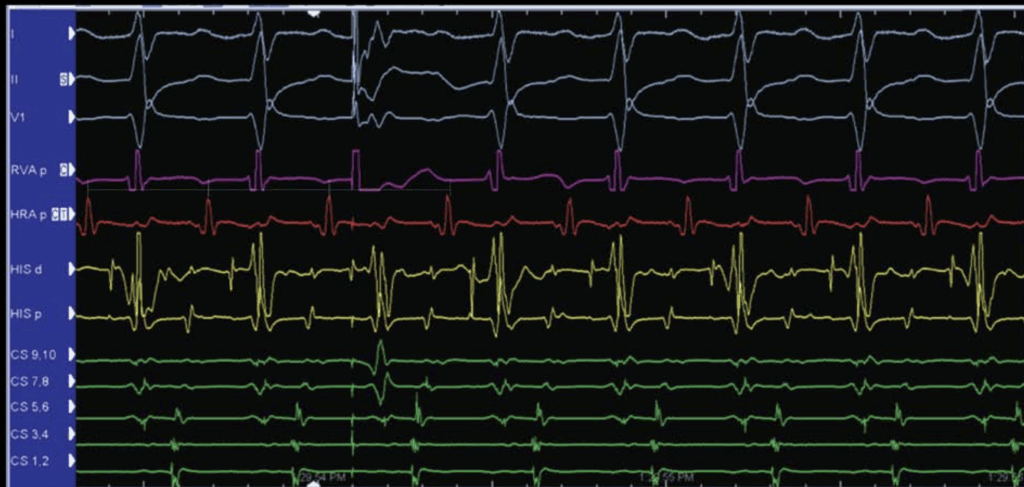
PVCs into AVNRT

Imagine you’re playing a game of tag inside a very tiny room—that’s exactly what’s happening inside your heart during AVNRT. In AVNRT, electricity loops in a tiny circuit within the AV node, causing your heart to race.
Now, during an EP study (think of it like a detective mission for heart rhythms 🔍), we use a clever trick to identify AVNRT clearly. We introduce a PVC (a premature heartbeat from the ventricle)—a bit like throwing a surprise ball into the game to disrupt the loop.
But here’s the catch! ⚠️
Because the AVNRT circuit is super small and hidden deep in the AV node, this surprise beat usually can’t break in to the tiny loop and change the rhythm above (in the atrium). So, the atrial rhythm stays steady, unaffected by our sneaky PVC.
Why do we even use a PVC then? 🤔
Good question! Even though it usually doesn’t affect the loop, introducing a PVC has a second, super handy purpose:
During AVNRT, the electrical signals from your atria (A) and ventricles (V) often overlap. It’s like two people talking at once—you can’t clearly hear who said what. By delivering a PVC, you briefly separate these signals—like hitting pause for clarity 🎧—making it easier to clearly see the atrial signals alone.
This way, we can precisely tell which area of the heart activates first. (His, CS ?) for the ablation strategy.
🌟 In short:
Introducing a PVC during AVNRT is like throwing a harmless distraction into a fast-moving game of tag. It helps us clearly identify the rhythm and safely plan our next move.
PVCs into AVRT
Imagine your heart rhythm as a relay race 🏃♂️💨. In AVRT, the electricity loops around a bigger track involving both your AV node and an accessory pathway (AP). Think of this AP as a secret shortcut pathway.
When we perform an EP study 🔍, we can introduce a PVC—a surprise extra beat from the ventricles—to see how your heart reacts. Because AVRT has a larger loop, the PVC can easily jump onto this bigger circuit and affect the rhythm of the atrium above.
What happens when the PVC is timed cleverly? 🕒
We deliver the PVC exactly when the AV node (specifically, the “His” area) is taking a brief nap (refractory period)—so it can’t respond. This tricky move is called a “His-refractory PVC”, and it helps detect if there’s a hidden shortcut (AP) involved.
Depending on your heart’s reaction, we learn different things:
No change (Atrium stays steady):
This doesn’t give much information. It could be AVNRT, or AVRT—it’s unclear. 🤷♂️Atrium beats earlier (“Advancing the atrium”):
This means your PVC used a hidden shortcut (the AP) to reach the atrium quickly! It’s like taking a secret tunnel. 🚇
It confirms you have a shortcut, but doesn’t confirm yet if it’s actively involved in the tachycardia.Atrium beats later (“Delaying the atrium”):
This tells us that your shortcut (AP) slowed down because of the PVC. It’s proof your shortcut is an active participant in your fast heartbeat race. 🐢The fast heartbeat suddenly stops! (“Terminates tachycardia”):
If a PVC causes your rhythm to stop without even affecting the atrium, it proves your fast heartbeat was AVRT. The PVC essentially blocked the shortcut pathway, ending the race entirely. 🛑🏁
🌟 In short:
Introducing a clever PVC during AVRT is like placing obstacles on a relay race track to see if runners use secret shortcuts. This helps us uncover exactly what’s causing the fast rhythm and guides effective treatment.
🎶 Entrainment Pacing – Keep the Rhythm Fun!
Imagine your heart rhythm is like a group of dancers spinning around in a big circle (this is called macroreentrant tachycardia 💃🕺). We want to know exactly where these dancers are spinning, so we use a special trick called entrainment pacing.
🎵 How does Entrainment work?
We pace the heart slightly faster (only a tiny bit, like turning the music tempo up just a little 🎧). The heart rhythm (the dancers) follows this new beat temporarily. When the we suddenly stop pacing, the heart quickly returns to its original fast rhythm—but the important clue is how fast it returns.
🕑 Timing Matters – The “PPI” Trick
We look at something called the Post-Pacing Interval (PPI). It’s basically how long it takes for the heart to return to the original rhythm after pacing stops:
If the catheter (the pacing source) is close to the dancers’ circle:
The dancers immediately jump back into their rhythm.
The PPI is short (close to the normal tachycardia cycle length, TCL).
If the catheter is far away from the circle:
The dancers take longer to get back into their groove.
The PPI is longer (much bigger than the TCL).
🔍 Example: AVNRT vs AVRT
AVNRT: The circuit is small and hidden deep in the AV node.
Pacing from a far-away spot (like the right ventricular apex) leads to a longer PPI.
(It’s like trying to influence dancers from across the dance hall!)
AVRT: The circuit is bigger, involving the atrium, AV node, ventricle, and a shortcut pathway.
Pacing from the same spot results in a shorter PPI because you’re pacing closer to the dance circle itself.
We often use a simple rule to decide:
PPI minus TCL >115 ms: Likely AVNRT (far from pacing spot).
PPI minus TCL <115 ms: Likely AVRT (close to pacing spot).
🌟 In short:
Entrainment pacing is like briefly turning up the tempo of music to see how quickly dancers respond. It helps us figure out exactly where the rhythm issue is and guides us to the best treatment!
🎯 Para-Hisian Pacing
Imagine your heart as a busy city with different roads for electricity to travel. Usually, the path through the AV node is the main highway 🛣️. But sometimes there’s a sneaky shortcut—a hidden road called an Accessory Pathway (AP).
When this shortcut is far from the center (septum), we can easily see it, because the electric signals look obviously unusual. But when it’s close to the center (near the AV node), it’s hard to know if the electricity is using the regular AV node or taking the sneaky shortcut.
To figure this out, we invented a clever trick called “Para-Hisian pacing.”
🔎 How does Para-Hisian Pacing work?
We pace the heart from an area very close to a structure called the His bundle (the main electric highway). They do it in two clever steps:
Step 1 – High Power ⚡ (His Bundle Capture):
We pace with high power to activate the His bundle directly.
Think of it as directly driving onto the main highway.
Result: A narrow QRS (normal-looking ECG), and electricity quickly moves backward to the atrium (short V-A time).
Step 2 – Lower Power 🔋 (Only Myocardium Capture):
Now we lower the power just enough so they don’t activate the His bundle, but still activate the nearby heart muscle (myocardium).
Think of this as driving through slower, side streets instead of the highway.
Result: A wider QRS (looks different), because electricity slowly travels through regular muscle.
🕑 Why does timing matter?
We measure the time from the pacing stimulus to the atrium (V-A interval) during both steps:
If NO shortcut (No AP):
High-power pacing (His bundle capture): short V-A interval (quick return).
Low-power pacing (muscle-only capture): longer V-A interval, because the electrical signal must travel through the entire ventricle to reach the AV node and atrium (like taking a long detour 🚗).
Difference between high-power and low-power pacing: about 45-50 ms.
If a shortcut (Septal AP) IS present:
Low-power pacing still results in a short V-A interval, because the sneaky shortcut lets the signal quickly jump back to the atrium—avoiding the long detour!
Difference between high and low pacing is much smaller because the shortcut saves time ⏱️.
🌟 In short:
Para-Hisian pacing is like testing two routes in your heart—taking the fast highway (His bundle) and a slower road (myocardium). By comparing these two trips, doctors discover if there’s a hidden shortcut nearby.

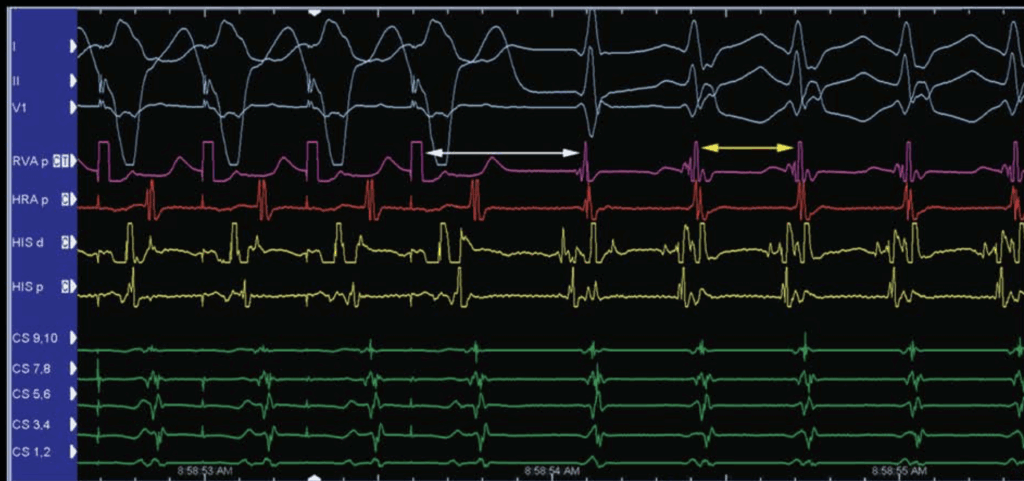
Normal Para-Hisian Pacing

Here you notice that the VA timing are identical -> Septal accessory pathway