Clinical Supra-Ventricular Tachycardia
Tachycardias Unplugged: When Your Heart Goes in Circles!
We start with the basics :
AV Nodal Reentrant Tachycardia
Atrioventricular Reentrant Tachycardia
Atrial Flutter
Atrial Tachycardia
1.0 - AV Nodal Reentrant Tachycardia
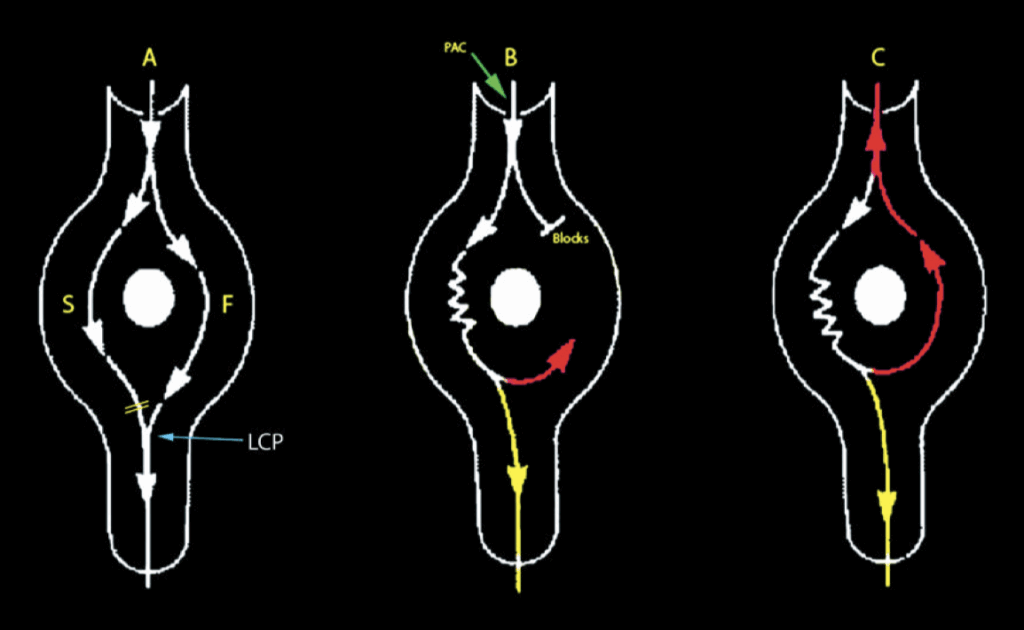
Typical AVNRT Pathways
Think of AVNRT (AV Nodal Reentrant Tachycardia) as a quirky rollercoaster ride inside your heart’s electrical system. Normally, signals smoothly glide down one pathway, but in AVNRT, there’s a fun twist: two pathways exist—a fast track (F) and a slow track (S). we call this setup “dual AV nodal pathways.”
Panel A: Imagine two paths through a park: one is a fast, smooth sidewalk (Fast pathway), and the other a winding, leisurely trail (Slow pathway). Usually, your heart prefers the sidewalk—it’s quicker. The electric wave quickly races down the fast track, activating your ventricles (the bottom chambers of the heart). The slow track also carries signals, but by the time they arrive, the Lower Common Pathway (LCP) is already busy and won’t let them through.
Panel B: Now, imagine someone suddenly throws in an early beat (premature atrial contraction, or PAC). This is like someone unexpectedly blocking your usual fast sidewalk. Since the sidewalk (fast path) isn’t ready yet, your heart’s signal takes the slow, winding trail instead. Because of this detour, the travel time suddenly becomes longer—we notice this as a sudden increase (or “jump”) in your heart’s electrical intervals (A-H interval). As the signal leisurely travels down the slow pathway, the previously blocked fast pathway finally recovers and opens up again. The electric signal then cleverly sneaks backwards up the fast pathway (red arrows in Panels B and C).
Panel C: And voilà—this forms a loop! The electric signal continuously spins around, down the slow path, then back up the fast path, repeating again and again. Your heart now experiences a rapid loop, leading to AVNRT, a fast but typically harmless heart rhythm.
This explanation is a simplified model—like a cartoon map of the heart’s electrical adventures. In reality, the exact structure of these two pathways is still a bit of a mystery, and we suspect variations in how these paths connect. Interestingly, when we perform procedures to stop AVNRT (ablation), we typically target the slow pathway near the coronary sinus opening.
Think of it as strategically closing off the slower winding trail in the heart’s park, forcing the electrical signals back onto the quicker, more efficient sidewalk path.
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
1.1 - The AV Node’s "Jump"
When performing extra-stimulus testing (the famous S1-S2 protocol), you keep measuring the A-H interval (the time it takes signals to cross through the AV node). Initially, the fast route handles traffic smoothly, but as you push it with increasingly premature beats (shortening S1-S2 interval), this fast highway gets tired, slows down gradually, and eventually closes temporarily (ERP reached).
Suddenly, your signals must divert to the scenic slow path. This sudden switch makes your A-H interval jump abruptly, becoming noticeably longer. Imagine cars suddenly forced off a highway onto a winding country road—traffic gets slower instantly!
We typically call this abrupt increase—a “jump“—significant if the A-H interval suddenly lengthens by at least 50 milliseconds with just a 10-millisecond reduction in the S1-S2 interval.
Why the Jump Matters:
This jump means you’ve clearly shown “dual AV nodal physiology,” the setup necessary for AVNRT to occur. Typically, this slow path results in pretty long A-H intervals—anywhere from 250 to 700 milliseconds or more.
Clinical Insight (Fun Facts):
Interestingly, just having two AV nodal paths doesn’t guarantee AVNRT.
Similarly, AVNRT sometimes occurs even without seeing a clear jump.
Sometimes, getting the AVNRT party started can be challenging. You might need extra “nudges”:
Using multiple extra-stimuli (S2-S3 or more).
Pacing from different locations.
Giving medications like Isoproterenol or Atropine can help “spark the rhythm” by speeding up conduction.
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
1.2 - AV Nodal Echo : Your Heart's Sneaky Boomerang
Before our heart jumps into full-blown tachycardia, we often notice a curious phenomenon: the AV nodal echo. Think of this as your heart’s electrical version of a boomerang—it’s a beat that cleverly loops back to exactly where it started.
What’s an AV Nodal Echo?
When we pace the atrium, we typically see a nice and predictable response: pacing the atrium (A) leads to ventricular activation (V). Everything is neat and tidy. But sometimes, the heart surprises us:
After several normal paced beats (S1), we deliver a premature beat (S2). This beat follows the usual route down to the ventricles, but then—surprise!—another atrial signal (A) unexpectedly appears. It’s as if our signal decided to turn around and return home (to the atrium).
We call this sneaky return an “echo beat,” essentially a single loop of AVNRT.
Breaking It Down (Simply):
Beats 1-3 (S1): Short and stable A-H intervals (fast pathway working smoothly).
Beat 4 (S2): A suddenly longer A-H interval, indicating a switch to the slow AV nodal pathway (the fast route is blocked temporarily).
This signal then loops back retrogradely (upward) to the atrium, creating our echo beat.
Why Doesn’t the Rhythm Keep Going?
(Un)Luckily for us (and our patients!), this particular echo doesn’t keep looping continuously into sustained AVNRT. After the echo returns, the slow pathway decides not to carry the next beat forward—it blocks conduction forward again, preventing a sustained rhythm.
Think of this as your heart politely declining to keep the “echo party” going after just one dance!
Quick Clinical Tip (We love this part!):
The presence of an echo beat hints clearly at the dual AV nodal pathways setup.
These echo beats can tease us, showing potential for AVNRT without fully kicking off a sustained rhythm.
They are useful markers during electrophysiology studies to confirm we’re dealing with typical dual-pathway physiology.

Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
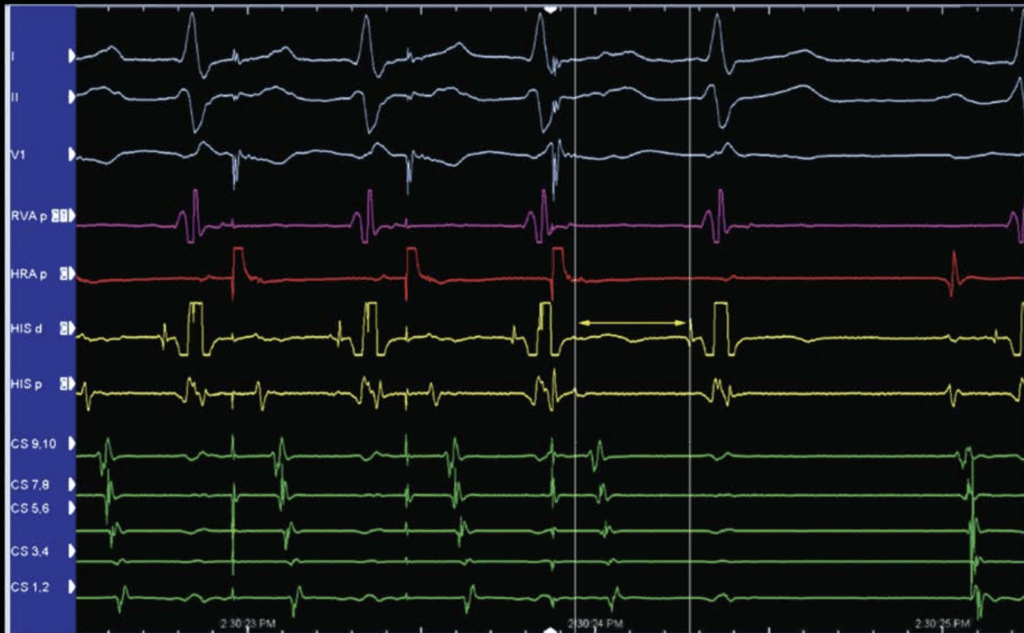
1.3 - AVNRT Onset Made Easy (and Entertaining!)
Step-by-Step Onset:
The Scene: Your heart normally beats calmly, sending signals smoothly through its electrical pathways. On the screen (electrogram), you notice a regular rhythm with beats nicely paced apart (drive train).
Suddenly—a Surprise Beat (S2)!
Imagine someone accidentally stepping on your dance partner’s toe (the red beat labeled S2). This unexpected beat doesn’t follow the usual pathway (the fast route is temporarily busy or “blocked”), so it takes a detour via the slow route. This slow detour appears as a long pause (flat line on your screen)—like your signal slowly tiptoeing through a winding corridor (the slow pathway, yellow arrow).Finally, the Signal Arrives!
After this long pause, the signal finally reaches the bottom of your heart (ventricles). On the electrogram, you’ll see an H spike followed quickly by a V spike (representing the activation of the ventricles).The Sneaky Return Trip:
Now, here’s where it gets fun! While your signal heads to the ventricles, it also sneaks back upward to the atria (upper heart chambers) through the now recovered fast pathway (red arrow). This creates a quick backward activation (retrograde conduction), seen on your screen as another atrial spike (red A) just below the ventricle signal (magenta V).
Echo Beats—The Repeat Dance:
If your signal does this sneaky loop once or twice, we call these “AV nodal echo beats“—like echoes bouncing around your heart.
But if this loop continues repeatedly, your heart rhythm takes off into a full-blown AVNRT dance party (fast heartbeat!).
Typical “Slow-Fast” AVNRT:
We call this the “slow-fast” or “typical AVNRT” because the signals move slowly down one pathway and quickly zip back up another. It’s the most common AVNRT rhythm doctors encounter.
Stopping the Dance Party—Ablation:
The good news is that we can fix this rhythmic dance by gently blocking (or ablating) the slow pathway—the essential slow corridor your signals use.
But there’s an important catch: the slow pathway is very close to your heart’s main electrical hub (the AV node).
Imagine carefully turning off music at a party—do it too abruptly, and everything stops suddenly (complete heart block).
That’s why we perform this procedure with extreme care and precision—keeping everyone safe on the heart’s dance floor!

Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
2.0 - Atrioventricular Reentrant Tachycardia

🎢 AVRT – The Heart’s Rollercoaster Ride!
Imagine your heart is a city with roads (electric pathways) guiding traffic (electric impulses) smoothly from one place to another. Usually, there’s one main road—the AV node—linking the upper city (atria) to the lower city (ventricles).
But sometimes, your heart has a sneaky extra road, called an Accessory Pathway (AP). It’s like a secret shortcut that wasn’t supposed to be there, creating some traffic adventures we call AVRT!
🌍 Where Do We Find These Secret Shortcuts?
Accessory pathways (APs) can pop up anywhere around the border (AV ring) between the atria and ventricles:
On the right side
On the left side
In the middle (septal) or near the AV node (peri-nodal)
These secret pathways can send electric signals either:
🔽 Downward only (atria ➡️ ventricles)
🔼 Upward only (ventricles ➡️ atria)
🔄 Both ways! (most common scenario)
⚡ Pre-Excitation – The Sneaky Early Start!
If the AP lets signals travel downward (antegrade conduction), it can make the lower heart chambers (ventricles) get excited too early. Think of it as your heart jumping the gun in a race. Doctors call this “pre-excitation.”
On an ECG (the heart’s electrical selfie 📸), pre-excitation looks like a little bump at the start of the QRS wave. Doctors call this a “delta wave”—a tiny curve telling us, “Oops! Someone took a shortcut!”
Sometimes the delta wave is very clear, like an obvious shortcut.
Other times, it’s subtle, like a sneaky little detour you hardly notice.
🕵️ Concealed Pathways – The Hidden Roads
Some APs only let electricity travel upward (retrograde). These are like hidden roads because there’s no delta wave on the ECG—so they stay secret and concealed. No one knows they’re there until they cause trouble!
When these hidden pathways get involved, signals usually go:
Atria → AV node → Ventricles → sneaky AP → back to Atria
This forms a nice circular race we call “Orthodromic AVRT”, usually showing a narrow (skinny) QRS on the ECG.
🔄 Antidromic AVRT – Reverse the Rollercoaster!
If the AP conducts signals downward only (antegrade-only), the race takes an opposite route:
Atria → AP → Ventricles → AV node → back to Atria
This reverse direction creates a wide (fat) QRS on the ECG. Doctors call it “Antidromic AVRT”—the backwards rollercoaster ride. This one’s less common but interesting!
🔁 Bidirectional Pathways – Two-Way Streets!
Most APs are two-way streets, meaning signals can zoom both ways. They can create either:
Orthodromic AVRT (skinny QRS, more common)
Antidromic AVRT (wide QRS, less common)
The heart gets to choose its adventure!
🎲 Rare Fun Fact!
Sometimes (in about 5% of cases), a heart has more than one secret pathway. Then, you can get a really special tachycardia where signals avoid the AV node completely!
The electric impulse takes:
Atria → AP #1 → Ventricles → AP #2 → back to Atria
This creates a wide QRS tachycardia that’s pretty rare but very interesting. It’s like the heart is juggling two shortcuts at once!
🗝️ Summary:
Accessory pathways: Secret shortcuts causing extra heartbeats.
Orthodromic AVRT: Narrow QRS, common, hidden pathways or two-way streets.
Antidromic AVRT: Wide QRS, rare, pathways conducting downward.
Multiple APs: Rare and special—signals might skip the AV node entirely!
Now you’ve mastered AVRT in a fun and easy way! 🎉🚗💨
2.1 - Accessory Pathway Echo
🎤 Accessory Pathway Echo – The Heart’s “Sound Check”!
Think of your heart rhythm as music: usually steady and predictable 🎶. But sometimes, when doctors test the heart with special electrical signals (called programmed extra-stimuli), we see a special beat pop up—a little echo beat. It’s like your heart doing a quick “sound check” 🎤 before starting a full-blown concert (tachycardia).
🔎 What’s an Echo Beat?
An echo beat is like one complete loop around a circular track (reentrant circuit). It happens once and then usually stops—but sometimes it might kick off continuous loops (tachycardia).
Imagine pacing (stimulating) your heart from the ventricle (lower chamber). The electricity moves from the ventricles up to the atria (upper chambers) using our sneaky shortcut called the Accessory Pathway (AP).
🌪️ Tracking the Echo – Follow the Path!
Let’s picture exactly what happens step-by-step:
Stimulus in the ventricle (S2) 📍
Impulse moves upward through the AP 🔼, making the atria excited in an unusual direction (eccentric activation).
This tells us the AP is on the left side.
On our screen, CS 1-2 lights up first, confirming the AP location.
The impulse reaches the atria (A), and from there it heads back down again, but this time using the normal AV node (probably a slow pathway)—that’s why we see a long pause (long A-H interval ⏳).
The impulse then goes back down to the ventricles (V)—completing one full circle 🎡.
Surprisingly, the impulse even tries one more time going back up to the atria using the AP again (this is the extra half-cycle), but then stops!
🚦 Why Did the Echo Stop?
In our scenario, the echo beat didn’t lead to a full tachycardia loop (continuous racing heartbeats). Why not?
Because one part of the circuit wasn’t strong enough to keep the rhythm going. We call that weak point the “WEAK LINK.”
In this example, the weak link was the AV node—it blocked the impulse, stopping the echo from turning into sustained tachycardia 🚧🛑.
💡 How to Fix the Weak Link?
Sometimes doctors give medication (isoproterenol) to strengthen the AV node. Think of it like giving the AV node an energy drink! ⚡ This can help overcome the weak link, and the echo might then initiate a full-blown AVRT.
🎉 Summary (The Simple Version!):
Echo beat: Quick practice loop around a circuit involving AP and AV node.
Accessory pathway: Sneaky shortcut letting signals move up quickly.
Weak link: Usually the AV node, stops echo from continuing.
Isoproterenol: Can strengthen the weak link, potentially starting full AVRT.
Now you know how the heart tests out its secret pathways with these little echo beats before deciding if it’ll turn into a real tachycardia show! 🎶❤️😄
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
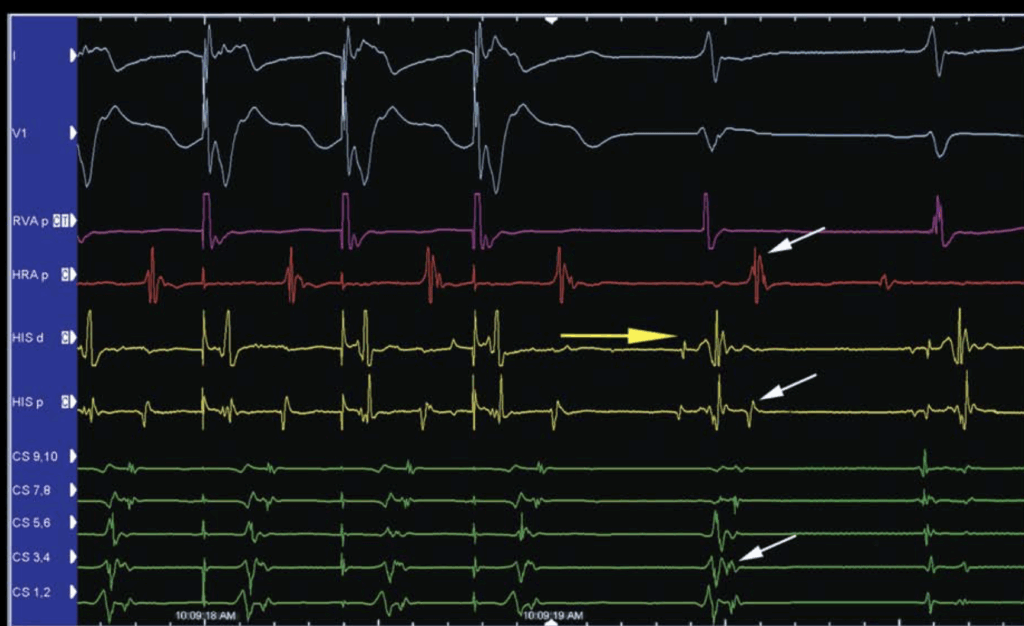
2.2 - 🏁 Starting the AVRT Race!
Picture your heart as a racing track 🏎️. Normally, electric signals cruise smoothly through the AV node—your heart’s main “traffic light.” But with AVRT, a sneaky shortcut (Accessory Pathway (AP)) lets these signals create a looping race track, causing your heart to beat extra fast!
🚦 How Does AVRT Begin?
For AVRT to start, signals need two roads:
Slow road (usually the AV node, yellow arrow 🟡).
Fast shortcut (our friend, the AP, green arrow 🟢).
Let’s walk through step-by-step how this racing loop kicks off:
Slow Start through AV Node 🐢
First, signals travel very slowly through the AV node (noticeable by a long A-H interval). It’s like the signal is taking its sweet time, stuck in slow traffic!
Fast Back Road via the Accessory Pathway 🚗💨
After the signal finally reaches the ventricles, it quickly zips backward (retrograde) through the AP up to the atria. This AP is located on the left side (near CS 1-2).
Eccentric Atrial Activation ↪️
Normally, signals activate the atria from right → left. But here, it’s reversed—left → right—because our sneaky shortcut (AP) is on the left side. We call this unusual pattern “eccentric activation.”
On our monitors, we see signals firing first at CS 1-2 (left atrium), then spreading across the atria (CS 3-4, CS 5-6, CS 7-8, then HIS A, and finally HRA A).
🔄 The AVRT Loop (Orthodromic AVRT)
The loop forms a circuit:
Atria → AV node (slow, yellow arrow 🟡) → Ventricles → AP (fast, green arrow 🟢) → Atria
This loop continues around and around, creating fast heartbeats known as Orthodromic AVRT.
🔍 Interesting Side Note:
Sometimes, you might notice no pre-excitation (no delta wave) on the ECG. Why?
Either because the pathway only conducts backward (retrograde),
Or the heart’s pacing speed hits the limit (Effective Refractory Period) of the AP, meaning it’s temporarily “closed” to downward (antegrade) conduction at that rhythm.
✨ Summary (Quick and Easy!):
AVRT initiation: Slow AV node conduction → Fast AP conduction (creates loop).
Eccentric activation: Signal travels backward, left → right atrium.
Cure: Ablation of the sneaky pathway stops the loop permanently.
Now you’ve easily understood how your heart starts racing around its special AVRT loop—and how doctors help calm things down again! 🎉💓

Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
2.3 - AVRT: Taking a Detour! (Bundle Branch Block Scenario)
Imagine your heart’s electrical system as a city with two main highways (bundle branches)—one going left (left bundle) and one going right (right bundle). Usually, electrical signals cruise smoothly down these highways, rapidly activating your ventricles.
But what happens if one of these highways gets blocked? 🚧
🚗💨 How the Detour Starts AVRT:
In this special scenario, the doctors give a carefully timed extra heartbeat (S2). This heartbeat takes an unusual route:
The Extra Beat (S2) and the Blocked Road 🛣️🚧:
The extra beat (S2) heads down to the ventricles, but it finds the left highway (left bundle) temporarily closed (in medical terms, Left Bundle Branch Block or LBBB).
Because of this block, the electrical signal must take a detour—it travels down the right side instead.
Slow Detour Across the Heart 🚙🐌:
After traveling down the open road (right bundle), the signal slowly moves through the heart muscle itself (trans-septally from right to left).
This slower journey through the heart muscle (instead of the usual fast highway) delays the signal significantly.
Delayed Signal Activates the Pathway! ⏳🎯
By the time the delayed signal finally reaches the sneaky left-side shortcut (Accessory Pathway or AP), the pathway has fully recovered and is ready to send the impulse back up to the atria.
This backward conduction through the AP starts the AVRT circuit, causing the heart to speed up!
Why Does this Happen Only on the Same Side (Ipsilateral)?
This type of AVRT initiation only happens if the blocked highway (bundle branch block) is on the same side as the Accessory Pathway:
Left-side AP + Left Bundle Branch Block (LBBB) ✅
Right-side AP + Right Bundle Branch Block (RBBB) ✅
If the blocked bundle branch is on the opposite side (contralateral) to the AP, no special detour occurs, and the pathway doesn’t activate. For example:
Right Bundle Branch Block (RBBB) will not initiate AVRT with a left-side AP. 🚫
🔄 Quick Scenario Recap:
Normal: Signals travel fast via bundle branches, no AVRT.
Blocked Highway (LBBB or RBBB): Forces a slow detour through muscle tissue.
Delayed Arrival: AP has enough time to recover and starts AVRT.
💡 Easy Summary:
Bundle branch blocks (blocked roads) cause slow detours.
Slow detours delay signals, giving AP time to recover and initiate AVRT.
Must match AP side (left AP with LBBB, right AP with RBBB) to initiate AVRT.
3.0 - 🎡 Atrial Flutter – A Fast Merry-Go-Round!
Imagine atrial flutter as your heart’s upper chambers (atria) spinning quickly like a merry-go-round, reaching around 250 beats per minute! This spinning is due to an electrical loop (reentrant circuit) that continuously goes round and round in the right atrium.
🗺️ Where’s the Loop? Meet the CTI!
This electric loop often passes through a small pathway called the Cavo-Tricuspid Isthmus (CTI)—imagine this as a narrow bridge or a tiny passage between two big landmarks:
The Inferior Vena Cava (IVC) (a large vein bringing blood back to the heart).
The Tricuspid Valve (doorway between the right atrium and ventricle).
This tiny bridge (CTI) is essential for the flutter loop. So we often target this spot to stop the flutter.
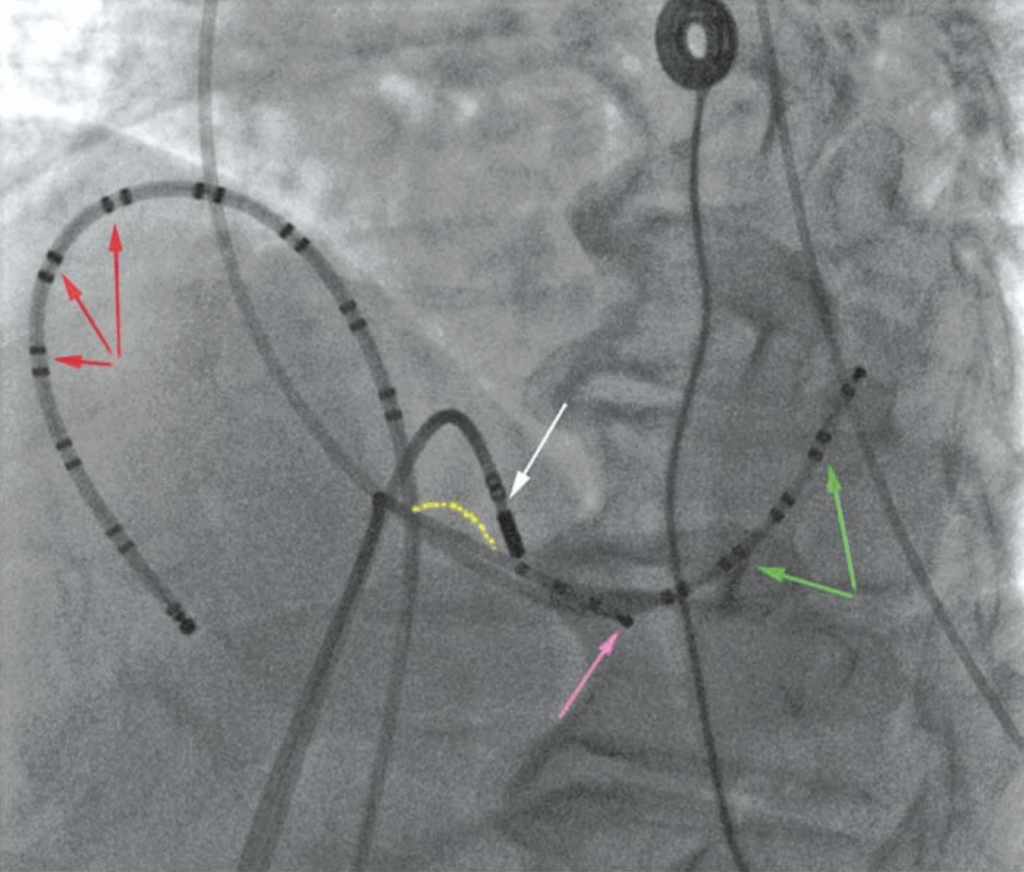
📌 How Do We Fix It? Catheter Placement!
We catheters to map and treat the flutter. Each catheter has a special purpose:
🔴 Duo-decapolar Catheter
Has many tiny sensors placed around the right atrium, positioned in front of a landmark called the Crista Terminalis (a muscular ridge).
Its job: track exactly how the electrical signal moves around your atrium.
⚪ Ablation Catheter
Positioned exactly on the tiny bridge (CTI).
Its job: deliver a bit of heat (radiofrequency) to create a small barrier, blocking the flutter loop permanently.
🟣 RVA (Right Ventricular Apex) Catheter
Placed in the ventricle to pace your heart if needed (like a backup pacemaker).
🟢 CS (Coronary Sinus) Catheter
Positioned in the coronary sinus (a vein around the heart) for pacing the atrium during procedures.
🎯 How Does the Ablation Work?
We slowly moves the ablation catheter from the tricuspid valve end toward the inferior vena cava end, creating a small line (like building a tiny wall 🧱) along the CTI (yellow dotted line).
This small barrier stops the flutter circuit, ending the fast merry-go-round 🎡.
🌈 Easy Color-Coded Summary:
🔴 Duo-deca Catheter: Maps electrical activity.
⚪ Ablation Catheter: Stops flutter at CTI.
🟣 RVA Catheter: Provides pacing backup.
🟢 CS Catheter: Used for atrial pacing.
📌 Why Proper Placement Matters:
Precise placement of the mapping catheter (duo-decapolar) is essential for accurate mapping. We use imaging tools (fluoroscopy or 3D mapping systems) to position catheters exactly right to understand and treat the flutter perfectly.
🥳 Quick Recap:
Atrial flutter: Rapid loop of electricity in the atrium.
Target: The CTI—tiny pathway critical to the loop.
Ablation: Creates a small barrier at the CTI to stop the loop.
Catheters: Placed strategically to map, pace, and ablate.
Now you’ve mastered the heart’s flutter treatment strategy—stopping that spinning merry-go-round and restoring a smooth, steady heartbeat! 🎉❤️🔧
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
3.1 - 🎯 Cavo-tricuspid Isthmus Ablation – Closing the Flutter Loop!
Think of atrial flutter as electricity running around your right atrium in a fast loop 🎡. The key to stopping this speedy merry-go-round is blocking one tiny road—the Cavo-tricuspid Isthmus (CTI)—a narrow strip of muscle connecting two key structures:
Tricuspid valve (doorway between right atrium and right ventricle)
Inferior vena cava (IVC) (large vein entering the heart)
Blocking this road prevents the electricity from looping around.
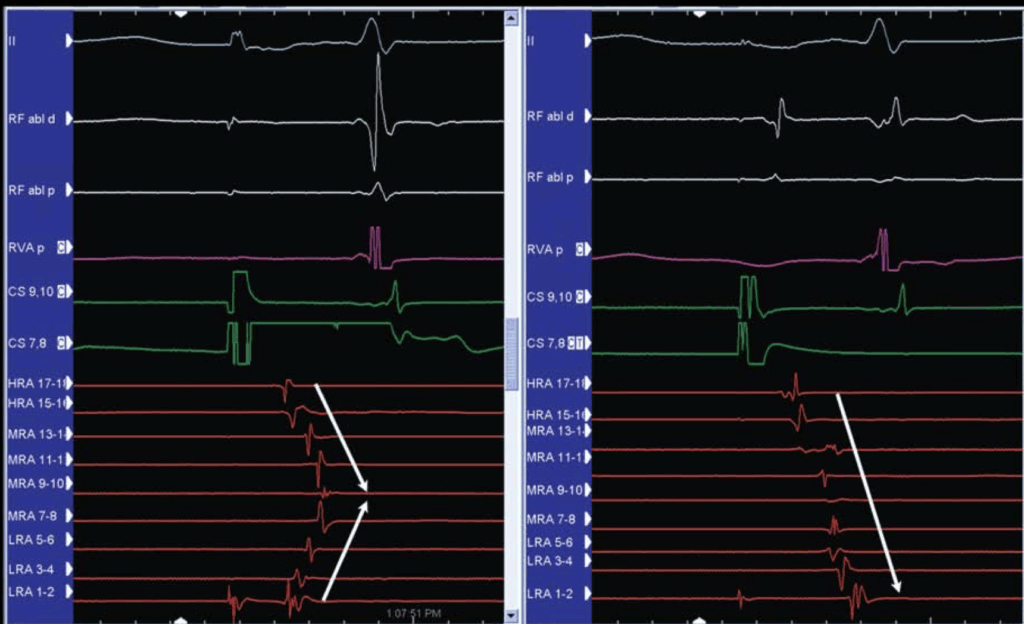
🔎 Testing the CTI – Before the Roadblock:
We first test if the CTI is open or closed by pacing (stimulating) your heart from different locations:
We place a special 20-electrode catheter (duo-deca) around the atrium to watch exactly how electricity moves.
Initially, we pace near the coronary sinus (CS) (a vein in the heart).
🌀 What Happens with an Open CTI (Before Ablation)?
The electrical signals travel along two separate paths:
One path across the CTI toward the lower right atrium (bottom path).
Another path moves up around the top (septum).
These two paths meet in the middle, creating a characteristic “chevron-shaped” (V-shaped ↘️↗️) wavefront pattern.
This V-pattern tells us the CTI is still open for conduction (signals can pass).
⚡ Performing the Ablation – Blocking the Road:
We then uses an ablation catheter to gently heat (radiofrequency energy ⚡️) and create a tiny barrier along the CTI.
After creating this barrier, we test again:
🚧 Testing the CTI – After the Roadblock (Ablation):
✅ What Happens After CTI Block?
If paced from de CS9-10, the electricity can’t travel directly across the CTI. Instead, it moves around the atrium in one smooth, single pathway (no more V-shape!).
The activation now starts at the top (HRA 17-18) and travels counter-clockwise around to the bottom (LRA 1-2last).
Additionally, the electrical signals at certain electrodes (LRA 1-2, 3-4, 5-6) flip their direction—proof that the pathway has been successfully blocked, forcing signals to go the opposite way around!
🔄 Bidirectional Block – Testing Both Directions:
To be certain the flutter loop is fully blocked, we test conduction in both directions:
From CS → LRA (clockwise) ✅
From LRA → CS (counter-clockwise) ✅
A successful block must be bidirectional (blocked both ways).
⏳ Timing Matters – Before vs. After Block:
Before block: Signal travels directly through the CTI (~80 milliseconds).
After block: Signal must take the long way around (usually doubling this time, ~160 milliseconds or more).
⚠️ Note: Sometimes signals can still slowly pass through the CTI, mimicking a block. We use multiple maneuvers to confirm complete blockage.
Simple Recap:
Goal: Block the CTI to stop atrial flutter.
Before ablation: Signals form a V-pattern (two-way conduction).
After ablation: Signals move around the atrium in one smooth direction (single-wavefront).
Final test: Confirm bidirectional blockage to ensure flutter is completely gone.
Now you understand exactly how doctors close that sneaky flutter loop—bringing your heart rhythm back to smooth sailing! 🎉❤️🚧
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
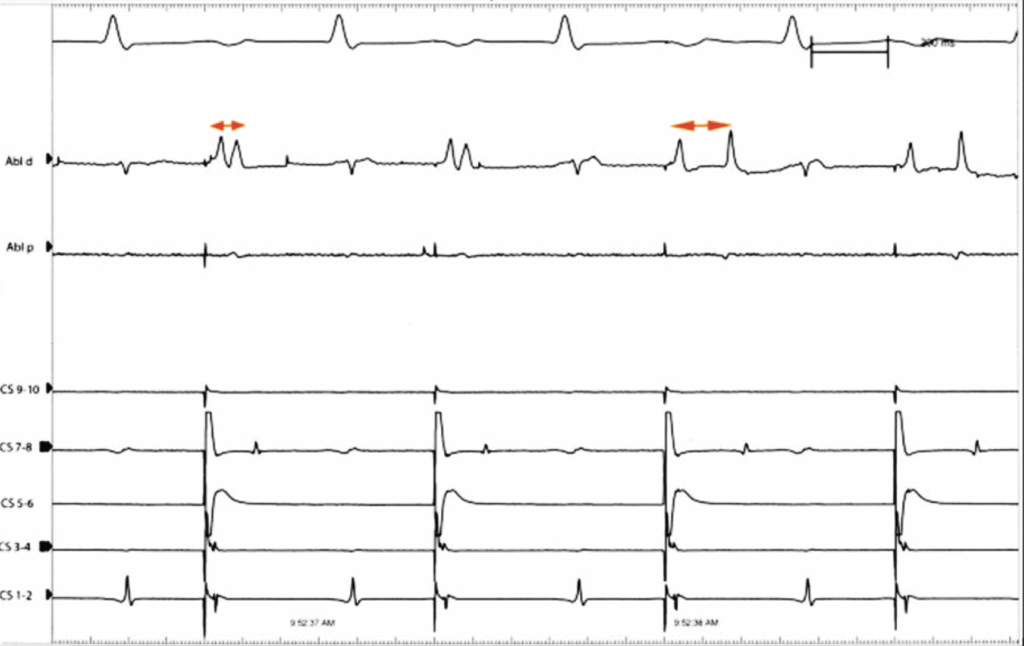
3.2 - 🎵 Split A’s – When One Beat Turns Into Two!
Imagine your heart’s electricity traveling smoothly, creating a single clear beat (“A-wave”). But sometimes during an ablation (procedure to block the flutter loop), this single beat splits into two separate beats—like a musical note suddenly turning into an echo 🎶🎶. This is what we call “split A’s.”
🤔 Why Does an “A” Split?
When we are ablating (blocking) the tiny bridge called the Cavo-tricuspid Isthmus (CTI), the electrical signals become confused as the bridge narrows or closes. The catheter’s electrodes can detect signals from both sides of the ablation line:
One side has early activation (quick arrival).
The other side has late activation (delayed arrival).
This creates two distinct beats on the screen—a split A.
🔥 What Happens During Ablation?
Initially, the split between these two beats is small because the electrical signal is still crossing the narrowing bridge (CTI)—just slowly due to tissue injury.
As ablation continues, this delay increases. Eventually, the signal can’t cross directly anymore.
Now, the delayed beat (late A) must travel the long way around the atrium (like a detour), dramatically increasing the split.
📏 Measuring the Split:
Small split (<80 milliseconds): Usually means the CTI is not completely blocked, signals still cross slowly.
Large split (>80 milliseconds, often >100 ms): Usually indicates complete block—the delayed signal is taking the detour around the entire right atrium.
🖥️ Example on Screen:
Early beats (beats 1 and 2): split is small (40 ms), indicating partial conduction through CTI.
Later beats (beats 3 and 4): split is bigger (140 ms), strongly suggesting full blockage of CTI.
🧐 Confirming Complete Block – “Differential Pacing”:
Since slow conduction can look similar to complete block, we use an extra test called “differential pacing”:
If they pace close to the blocked line (CTI):
With complete block: the late beat will arrive even later, increasing the split.
With slow conduction: pacing closer might reduce or minimally affect the split (signals cross directly over CTI).
This helps distinguish true block from just slow conduction.
🗝️ Quick Recap (Made Easy!):
Split A’s: One beat splits into two due to partial or complete blockage.
Short split: Small delay, signals slowly cross CTI.
Wide split: Large delay, signals take detour (suggesting complete blockage).
Differential pacing: Helps confirm total block vs slow conduction.
Now you know exactly why a single beat turns into two during atrial flutter ablation—it’s your heart’s electric rhythm getting creative! 🎉❤️⚡
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
3.2 -  Split A’s – When One Beat Turns Into Two!
Split A’s – When One Beat Turns Into Two!
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Purves, P. D., et al. (2020). Cardiac Electrophysiology: Guide for Nurses, Techs, and Fellows. Cariotext.
4 - 🎯 Focal Atrial Tachycardia – A Single Troublemaker!
Imagine your heart’s rhythm is usually like a symphony, with signals smoothly coordinated. But sometimes, a small, rebellious area in one of your atria decides to beat faster on its own—this is called Focal Atrial Tachycardia (Focal AT). Think of it as a tiny drummer playing faster than the rest of the orchestra, making the rhythm chaotic! 🥁🎶
📍 Where Does Focal AT Come From?
Focal AT starts from one tiny spot (a “focus”) in the left or right atrium.
Unlike AVRT or AVNRT (that use loops or extra pathways), this tachycardia comes from one little misbehaving spot (pink star ⭐️).
🧩 Challenges in Ablating Focal AT:
Focal AT can be tricky to treat for two main reasons:
1️⃣ Difficult to Trigger:
We must first get the tiny troublemaker to show itself in the lab.
Sometimes it appears spontaneously, but other times it needs encouragement (like special stimulation or medications such as isoproterenol—think caffeine ☕️ for your heart!).
2️⃣ Harder to Locate:
Unlike other rhythms (e.g., AVNRT or WPW) where targets are predictable, focal AT must be mapped while it’s actively causing trouble.
We can only find and target this tiny spot during actual tachycardia.
🗺️ Finding the Spot – Activation Mapping:
To find the misbehaving spot, we perform Activation Mapping:
We create a detailed electrical map of your atrium during the rapid heartbeat.
We carefully find the very earliest signal—this pinpoint is where the troublemaker is hiding.
We often use special 3D electro-anatomical mapping systems, which show exactly where the fastest signals originate.
Additional Techniques:
Pace mapping and entrainment mapping can also help, but detailed activation mapping is usually essential.
🔎 How to Confirm it’s NOT Sinus Tachycardia?
Sometimes, we must make sure the fast rhythm isn’t just your heart’s natural pacemaker (SA node) speeding up (sinus tachycardia).
We perform a test called entrainment (briefly pacing close to the trouble spot):
If it’s focal AT, pacing very close creates a very short gap (<20 ms) between pacing and the actual tachycardia (PPI – TCL < 20 ms).
If it’s sinus tachycardia (SA node speeding), the shortest possible gap is around 80 ms or more because the SA node is “protected” from very close pacing.
🎉 Simple Recap (Easy Summary):
Focal AT: Fast heartbeat from one tiny spot in atria.
Hard to trigger: Needs encouragement to appear in the lab.
Activation mapping: Finds exact spot during active tachycardia.
Confirming focal AT: Short pacing gap confirms focal AT, while long gap (≥80 ms) indicates sinus tachycardia.
Now you understand exactly how doctors identify and handle that tiny rebel causing your heart’s rapid rhythm! 🎶⚡❤️
Some Random Notes
VA relationship :
- V = A -> AVNRT, AVRT, AT
- V < A -> AT, AVNRT (rarely)
- V > A -> VT
VA interval (RP) :
- Short RP : Ty AVNRT, AVRT, AT
- Long RP : Any AVNRT, AT, AVRT with slowly conduction AP
P wave morphology
- Retro P, negative P in DII, DIII, aVF -> AVNRT, AVRT, AT
- Positive P DII, DIII, aVF -> AT
ECG :
- Invisible P wave -> 65% AVNRT
- (in)visible P wave -> 30% AVNRT
- Visible P wave -> rare AVNRT/Slow-slow AVNRT, AVRT
Age & sex :
- Young + men -> AVRT ++
- Young + women -> AVNRT
- Older + men -> AVNRT
- Older + women -> AVNRT
Adénose response :
- AVNRT + AVRT ortho -> STOP
- Can terminate AT or Flutter
Baseline characteristics
- 12 ECG : pre-excitation ?
- Ventricular pacing & if retrograde conduction :
- Is it decremental ?
- Is it concentric ?
Tachycardia induction :
- Initiation of tachycardia
- AH prolongation
- Change in QRS
- Termination of tachycardia
- Characterics of tachycardia
- Cycle length
- Regularity
- VA < 70 ms (50 ms)
- Activation
Pacing manoeuvre :
- Ventricular overdrive pacing
- PVC on His refractory
- If non induction Isuprel
- Adenosine in sinus rythme
- ParaHisien pacing